We receive questions every day regarding the use of medical infrared imaging (MIR). Most of these questions are generated by the vast amount of misinformation found on the internet. MIR is an incredible technology with a great deal of good to offer the health of every person. However, this misinformation can lead to the misuse of this lifesaving technology. As health care professionals we are extremely concerned about what we are hearing and seeing.
Education is the ultimate answer to this problem. With quality education, founded in research and following accepted standards and guidelines, the proper application of MIR benefits everyone. With quality instruction comes quality thermal imaging.
We hope that the following will help to dispel the misinformation we see on the internet and bring about an understanding of how this lifesaving technology may benefit you.
Thermography Basics
What is thermography (medical infrared imaging)?
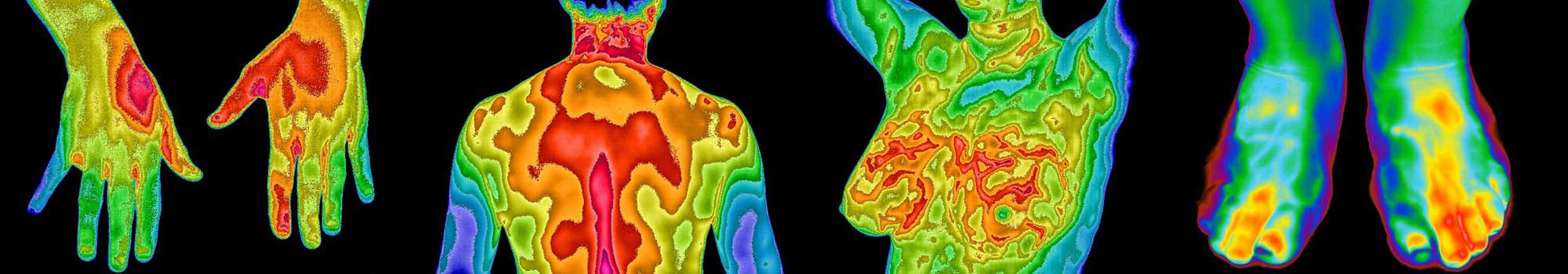
Thermography entails the use of specialized cameras that are sensitive to the detection of electromagnetic energy (light) in the infrared wavelengths (heat). As such, these imagers serve as a remote sensing system; nothing touches or harms the object under investigation. When the camera’s detectors sense the incoming infrared heat an electrical signal is produced that generates a visible image display.
Thermography, or infrared imaging, is used in numerous fields such as industrial fabrication, astronomy, building construction, military applications, surveillance, aerospace sciences, and of course medicine. Medical infrared imaging (MIR) entails the use of high-resolution infrared cameras and sophisticated computer processing to produce a topographic heat map display which bears a resemblance to the visible image of the body. Modern computerized thermography produces an accurate and reproducible high-resolution image that can be analyzed both qualitatively and quantitatively for minute changes in skin surface heat emissions.
MIR is applied in the clinical environment as an aid in the diagnostic process. It is used for the thermal analysis of patients with various conditions in acute, chronic, and preventative health care.
Is medical infrared imaging safe?
Yes! Infrared imaging (or thermography) uses no radiation or intravenous access and does not touch the body. The procedure is painless, completely safe, and FDA approved as an adjunctive imaging procedure (to be used in addition to other tests). Infrared imaging does not replace any other form of imaging (e.g. CT, MRI, mammography), but is designed to be used in addition to other tests to provide physiological information that cannot be obtained from any other examination procedure.
Is thermography experimental?
No! Based upon the available research data at the time, the U.S. Department of Health Education and Welfare (HEW) determined that thermography was beyond the experimental stage in 1972. Thermography was approved as an adjunctive imaging procedure by the FDA in 1982 (Federal Register, Vol 47, No. 20, pp 4419-4420, January 29, 1982). The FDA approved thermography as follows: “Telethermographic systems intended for adjunctive diagnostic screening for the detection of breast cancer or other uses” (Code of Federal Regulations – Title 21, Section 884.2980 Telethermographic Systems).
Do I need a referral from my health care provider?
You do not need a referral and may schedule directly with our center.
I have seen news releases that are very negative about breast thermography.
We have also seen this news. If you look closely you will find a common thread among all of these negative reviews; the procedure is being done incorrectly. When personnel are properly trained, and guidelines are strictly followed, breast thermography can be a lifesaving technology. And, like any other procedure in healthcare, what is the expected outcome if things are done incorrectly?
Is thermography a replacement or alternative to X-ray, ultrasound, MRI, CT or any other type of imaging?
No! The technologies are completely different. One cannot compare a functional imaging technology to a structural imaging tool. For example, an EKG does not replace an echocardiogram. The two technologies look at the heart in a completely different way, yet they complement each other. Thermography provides information about the body that no other technology can offer, but it does not replace them. The reason why there are so many different medical imaging technologies is because no one technology can do it all. They all have strengths and weaknesses.
Thermography does not replace any other form of imaging, but is designed to be used in addition to other tests to provide physiological information that cannot be obtained from other examination procedures. Thermography is an adjunctive physiologic imaging procedure that does not look inside the body. If you are interested in looking for structural changes such as broken bones, or viewing the colon, female reproductive organs, or the arteries of the heart, please see your doctor for the most appropriate test.
Does thermography replace mammograms?
Absolutely not! However, do mammograms replace thermography? The answer to this is also a resounding no; the two tests complement each other. Thermography is adjunctive, it is to be used in addition to other imaging technologies as part of a woman’s regular breast health care. The consensus among health care experts is that no one procedure or method of imaging is solely adequate for breast cancer screening. The false negative and positive rates for currently used examination tests (including thermography) are too high for the procedures to be used alone. However, thermography may pick up thermal markers that indicate the risk of cancers not detected by other tests. An abnormal infrared image is also the single most important marker of high risk for developing breast cancer in the future. It is thermograpy’s unique ability to monitor the abnormal temperature (physiological) and blood vessel changes produced by pathological breast tissue that allows for extremely early detection. Since it has been determined that 1 in 8 women will get breast cancer, we should use every means possible to detect these tumors when there is the greatest chance for survival. Adding these tests together significantly increases the chance for early detection.
Keep in mind that no one test or imaging technology can provide a warning for 100% of all cases. As such, all tests and imaging technologies are adjunctive. As an example, no doctor would tell a woman that all she needs is a mammogram and that she does not need to come in for her yearly physical breast exam. All doctors know that a certain number of breast cancers will be detected on a physical exam of the breasts and not detected on a mammogram. As such, a mammogram is also adjunctive – it must be used along with a yearly physical exam of the breast.
Another example of this “adjunctive” principle is the all too common experience of women having their yearly physical breast exam followed by their mammogram and then having to have a follow-up ultrasound to check on something seen on the mammogram. Now we are up to three “adjunctive” exams before a woman is told that everything looks fine. Now in some cases, if something needs to be watched on the mammogram and/or ultrasound, a woman might need to be called back in 6 months for another mammogram. Thermography might be the added technology that calls attention to something that needs a closer look.
It should be understood that all of these imaging technologies (thermography included) cannot tell you if you have breast cancer. They only provide a certain amount of suspicion based on what the individual technologies “see”. Only a biopsy can tell you if you have breast cancer.
There just isn’t one single magic bullet that will do it all. As such, the best approach to providing every woman with the best in early breast cancer detection is a multi-modal approach (multiple modality – multiple tests).
I have seen websites that say that thermography can detect problems with the stomach, colon, heart, immune system, female reproductive organs, prostate, and other internal organs.
The easy answer here is no. Thermography can only detect heat to a depth of 5mm from the surface of the body. As such, thermography cannot see into the cranial vault, thoracic cavity, abdomen, or pelvic basin. Remember the “visible man” model that was made for children? It had a clear plastic outer shell so that you could see the internal organs. With thermography, one cannot simply create a “visible man” image with heat at the surface of the body and think that you can transpose it to underlying anatomical structures. We have seen infrared images like this, but they are completely false and misleading.
Now, if an internal organ is damaged enough it may send a neural reflex message to the surface of the body creating an infrared marker (viscerosomatic reflex). This surface signal is rarely associated with the location of the underlying organ and is usually found in a remote location that only a well-trained board certified thermologist knows to look for. The problem is that by the time an internal organ is sending this signal there is usually a fair amount of damage. This viscerosomatic reflex can also burn out leaving no infrared marker. Combining this fact with an inability to offer an early warning means that thermography is also unable tell you that you are free of an internal disorder (rule out pathology). The technology is not sensitive enough to be used to screen for or rule-out internal disorders. There are much better tests and imaging tools that can provide for the early detection of pathologies of this type.
If you are concerned about a possible internal disorder, or the spread of cancer (metastasis), there are tests and imaging technologies that are better suited for this purpose. Please see your doctor for the most appropriate tests for your condition.
Choosing A Qualified Imaging Center
What do I look for in a qualified thermography center?
Choosing a qualified office or imaging center should be as simple as performing an internet search for an office in your area, but unfortunately it isn’t. There are many offices that have very poorly trained personnel using substandard imaging systems and doctors that are providing image interpretation without a proper education.
Just like any office or imaging center offering radiology services, a qualified thermography center should have certified technicians performing the imaging and a board certified thermologist providing the interpretation of the images. But are these “certified” technicians and “board certified” thermologists really well-educated and certified? This is the problem we are seeing. The caliber of the training of the technician and thermologist is of the utmost importance. I guess the best way to understand the current problems we encounter, and the solution to this problem, is to use an example that we can all understand.
I think that all of us could agree that Harvard University is a good example of a quality institution of higher learning. But how do we know this? Well, Harvard has a long history of providing an exceptional education through their well-educated faculty. And the students who graduate are a reflection of this level of education. The foundation of this level of quality education is lineage. The professor that is currently teaching was taught by a professor who also had this level of quality instruction and this professor also had ……… you get the point. Without a quality lineage of educators, you cannot produce a quality educated student.
Now it is up to you to ask the right questions when interviewing an office or imaging center providing thermography. Is the technician certified by an association or group that has a faculty that can trace their lineage? Does the technician provide imaging under recognized standards and guidelines? Has the thermologist providing their interpretations been board certified by a recognized group that can trace their lineage? Does the thermologist provide interpretation of breast thermograms using peer-reviewed and accepted guidelines – is each breast given a TH grading?
You will need to make the decision if the answer is no to any one of the above.
Are there standards and guidelines under which thermograms need to be taken?
In order to prevent artifacts on the images, every patient must be provided with a list of pre-imaging instructions that must be strictly followed. The imaging room must also be designed properly and environmentally controlled within strict guidelines. The room itself should be draft free and relatively cool (68-73 degrees F) with no incandescent lighting, no heat or cooling sources near the patient, no windows without coverings, and environmentally held steady within 1 degree C during the entire time of the imaging study. In other words, you should be placed in a draft-free cool room that is very thermally stable. You will also need to spend 15 minutes acclimating to the room before imaging (nude from the waist up for breast imaging or with suitable underwear and a loose-fitting gown for body imaging). And lastly, the imaging system itself must meet minimum acceptable specifications for medical use and be registered with the FDA in order to provide thermograpy. Without these standards in place the images would be useless.
I was told to come to a certain office because they had a better imaging system.
We find it sad that when providing a lifesaving service that some cannot put the patient first. Our policy is to always refer patients to the imaging center closest to them for their convenience. Using fallacious marketing practices that are designed to force patients into one’s own office is truly unacceptable. There are established thermography imaging system standards that need to be met in order for an imaging center to provide thermography. These standards were drafted in the 1980’s and have been recently validated and updated. Almost all quality modern infrared camera systems that are designed for medical use exceed the minimum standards for thermography. The most important issue here is the phrase “designed for medical use”. Unfortunately, there are companies that claim that their imaging systems are “designed for medical use”, but in reality they are far from it. There are quite a few technical aspects of infrared imaging that need to be met in order to accurately analyze the surface temperatures of the human body. Most infrared cameras are designed to meet the average needs for military uses, police surveillance, or industrial applications. The demands of a medical imaging system far exceed these applications. The question then remains, are there infrared imaging systems that just meet standards and others that far exceed them? Yes, but the question is are these exceptional systems better? In 2003, Dr. William Amalu, DC, DABCT, FIACT (Board certified clinical thermologist and executive board member of the IACT and ITS) was asked by the board of the International Thermographic Society (ITS) to investigate the need for a change in the imaging system standards. In other words, based on the quality of the newer imaging systems will offices and imaging centers need to retire their older equipment and purchase state-of-the-art imagers? At this point we need to be careful with what we are defining as quality in an imaging system. We need to be comparing apples to apples. The older equipment we are talking about was the state-of-the-art at the time and met every imaging qualification needed for accurate assessments of human infrared emissions. The newer imaging systems also meet or exceeded these standards along with a significant improvement in image quality. At the 2004 ITS symposium, Dr. Amalu presented his findings. He had gathered 100 patients totaling 200 image sets for analysis. Each of the patients had to have images taken on both 1980’s imaging systems and modern thermal imagers for comparison. He used the current interpretation guidelines to analyze all of the images. Dr. Amalu was able to demonstrate that offices and imaging centers using the older imaging systems did not need to update their systems to the state-of-the-art. Now does this mean that we don’t appreciate the significant improvements in image quality, ease of use, and reduced cost? No, of course we do. But to say to a patient that because your office has the latest and greatest that you are better than the office down the street is simply not true. Now, we have just made a comparison between apples and apples – older quality MIR imaging systems designed for medical use versus newer systems also designed for medical use. However, the real problem is that we are currently dealing with apples and oranges. Some companies and offices claiming that their imaging system is better actually have equipment that does not meet the requirements for medical imaging. Both the office using the equipment and the public have no idea that the images being produced may be completely inaccurate and a health risk. Here we come back to education. If an office or imaging center has a well-educated staff, you may rest assured that they will have a quality thermography system. Educational courses at this level have sufficiently covered both infrared physics and the design requirements needed when choosing an infrared imaging system meant for medical uses. As such, the imaging center will be adhering to established standards and guidelines. The current problem is that some health care offices and imaging centers are not sending their staff for proper training before they purchase an imaging system. Without the knowledge gained in a quality course there is no way an office or imaging center will be able to know the difference between a real infrared imaging system or a costly substandard camera.
Thermal Imaging Interpretation
What kind of doctor can provide interpretation of thermograms?
Within the healthcare specialties, DCs (Doctors of Chiropractic), MDs (Medical Doctors), and DOs (Doctors of Osteopathy) can become radiologists. Just as with radiology, DCs, MDs, and DOs can become thermologists. All of these doctors have the clinical acumen necessary to take additional training to specialize in radiology or thermology.
Are there standards and guidelines for the interpretation of thermograms?
Absolutely! How could any medical imaging technology provide service without standards and guidelines? Quality peer-reviewed and published research studies performed in leading universities have established a normative database of objective topographic thermal gradients and temperature values. Almost 10,000 references exist in the literature using this normative database to examine for pathology.
With regard to breast thermography, over 800 references exist in the literature to support the standards and guidelines under which breast thermograms are interpreted. All breast thermogram reports should contain a TH (thermobiological) grading of each breast. If a report does not grade each breast into one of 5 TH grades, the competency of the interpreting thermologist comes into question. The TH grading system was devised in order to provide a method for the universal interpretation of both qualitative and quantitative thermal data and to use this data to convey the level of risk and concern. Without a grading system there would also be no way to objectively monitor the progression of possible pathology or provide an objective indicator of improvement of the health of the breasts under care.
The TH grading system has been in place since the early 1980’s. The American College of Radiology (ACR) established the BIRADS (Breast Imaging Reporting and Data System) grading system for mammography in order to provide the same information when interpreting a mammogram, MRI, or ultrasound of the breast. The ACR states the following: “The BI-RADS provides standardized breast imaging findings terminology, report organization, assessment structure and a classification system for mammography, ultrasound and MRI of the breast. The report organization enables radiologists to provide a succinct review of mammography, ultrasound and MRI findings and to communicate the results to the referring physician in a clear and consistent fashion with a final assessment and a specific course of action.” Thermography uses the TH grading system to accomplish the same objectives.
When I get my report, will the thermologist provide me with treatment recommendations?
Absolutely not! It is the thermologist’s duty to NOT intervene in treatment. Your treatment must be directed by your doctor.
Does the thermologist know your complete health history? Has he or she reviewed all of your recent and past laboratory exams? Does the thermologist know all of the medications, supplements, herbals, etc. you are taking? Has the thermologist consulted with or at least have your complete health history from all the other health care providers/specialists involved in your care? Has the thermologist provided you with a recent physical examination to be sure of certain health markers? Can you imagine the level of irresponsibility the thermologist would have to undertake to make treatment recommendations simply off the findings of a thermogram? There is a real possibility here that a patient could be seriously injured or worse.
The findings and recommendations on the report are sufficient enough for your doctor to use in providing care. Have you ever seen a radiologist recommend anything other than further follow-up testing on a mammogram, X-ray, CT, ultrasound, or MRI report?
I’ve heard that there are computer programs that can read thermograms.
I think that we need to clarify this question first. If you are asking if there is an FDA approved computer program that will read the images and create a report without a board certified thermologist also reading the images, the answer is no. There is no place anywhere in health care where a machine provides interpretation of a test and creates a report without a doctor’s interpretation of the results. Have you ever seen a report from any imaging procedure that did not have a doctor’s signature (electronic or otherwise)? This is completely unacceptable in health care. Also, can you imagine the liability! No company would be foolish enough to want to accept this level of responsibility for their software program.
On the other hand, there are quite a few experimental programs currently being studied that are designed to aid thermologists when interpreting thermograms. However, we are not aware of any programs that have been proven to be accurate and approved by the FDA. As such, there is no adequate research proving that any of these programs are of value to the thermologist.
These programs are designed to work just like the FDA approved programs presently being used to aid radiologists when reading mammograms (e.g. ImageChecker).
On a side note, research has shown that the skill level of radiologists in detecting suspicious areas on a mammogram is far greater than that of the CAD programs designed to aid them. It’s nice to know that we humans are still better than machines.
I’ve been told that when doing a breast thermogram a cold-challenge must be done.
The use of the cold-challenge (placing the patient’s hands in ice-water, using ice mitts, or using ice packs placed on the mid-back) was stopped in the late 1980’s. The research at the time showed that using the cold-challenge did not increase the sensitivity or specificity of breast thermography. What we are finding is that some offices have websites telling women that they should never go to any office or imaging center that is not doing the cold-challenge. We have no idea why they are doing this as this is simply false information. Fortunately, the number of offices we see doing this is decreasing.
Back in the late 1990’s and early 2000’s the problem was so bad that Dr. William Hobbins (the leading expert in breast thermography at the time) encouraged Dr. William Amalu, DC, DABCT, FIACT (Board certified clinical thermologist) to review his database of cold-challenges and present a paper at the yearly symposium of the American Academy of Thermology (AAT). Dr. Hobbins and other experts in this field were concerned that these misleading offices were claiming that experts in this field were missing things by not performing breast thermography correctly. The paper went on to be presented at the international conference of the IEEE Engineering in Medicine and Biology Society. The end result was acceptance of the paper for peer-review and publication (click here or go to Medline/PubMed). As recently as 2013, the AAT formed a standards and guidelines committee that included Dr. Amalu, along with Dr. William Hobbins and a group of experts in this field, to review the current status of breast thermography and create an updated internationally peer-reviewed standards and guidelines document. With regard to the cold-challenge, a review of the literature along with a consensus among the experts reaffirmed that the cold-challenge did not improve the sensitivity or specificity of breast thermography; and as such, its use was not necessary to provide accurate infrared imaging of the breast.
New Cutting-Edge Thermography Systems
What about the new thermography systems I have heard of?
From time-to-time we see new thermography systems that make claims to significant superiority to the current imaging systems. What we find is that these systems are usually using methodologies that are untested and/or ignore the laws of thermodynamics. One of the most misleading of these “new” infrared imaging technologies is the claim of being able to look deep into the body. For a more detailed explanation, please see the first topic in the Thermography Myths section below.
Another problem we seeing is the use of imaging equipment in a manner that either introduces thermal artifacts or temperature measurement errors. This alone causes inaccurate data collection and interpretation errors. Another cause of errors comes in the form of unproven software interpretation programs that are used without a board certified thermologist interpreting the images. There is no place in healthcare where a machine provides an interpretation of a medical imaging procedure without a board certified radiologist or thermologist reading the images and signing the report (see previous topic above). Software programs such as ImageChecker (e.g. use in mammography) are used to assist the radiologist, but are not used alone.
The current infrared imaging system standards and interpretation guidelines have been established for over 34 years. These equipment and interpretation standards and guidelines have been continually monitored and updated by experts in this field through major associations worldwide. We are currently using the state-of-the-art in infrared imaging systems and interpretation methodologies. This involves infrared imaging systems that can withstand the scrutiny of the finest engineers in infrared sciences and the interpretation expertise from highly educated board certified thermologists.
I have heard that with certain newer imaging systems pre-imaging acclimation is no longer needed.
The sophistication of an infrared imaging system has nothing to do with human physiology. All patients must undergo 15 minutes of acclimation in an environmentally controlled room.
It doesn’t matter what type of imaging system you have, if you have been driving with your arm out the window and the AC blowing on the other side of your face you cannot be suddenly placed in front of a heat sensing camera to take images. When going from a hot environment to a cool one, and vice versa, the body needs to become attuned to the environment in order to express accurate thermal information. Clothing will also leave marks on the surface of the body (thermal artifacts) that have to be removed before imaging can take place.
You could have the most accurate and sensitive thermometer in the world, drink a hot cup of coffee and stick the thermometer in your mouth. Do you think that you would get an accurate representation of temperature?
Thermography Myths
I’ve heard of a new advancement that allows infrared imaging to see deep into the body to detect tumors, organ pathologies, and other deep structures.
There is nothing new here. These claims were made in the 1990’s, 2000’s, and now again. Every time this has occurred no one has ever been able to prove it. They will tell you that research has been done. They will show you images that claim to prove that their system is the only one that can do this. In most of these instances what you are being shown is common digital subtraction methods that are built into all quality imaging systems.
In all of these instances basic research studies have never been replicated. We know that thermography can only see to a depth of 5mm. How do we know this? Research studies were performed long ago using both animals and humans. Multiple volunteers had heat generating modules surgically implanted at varying depths from the bone to the surface of the skin. The surgical procedures were allowed to completely heal and baseline MIR images taken to demonstrate normal thermal patterns. Each module was turned on individually and heated to just under the point of causing cellular death (This is well over any temperature that would be generated from a pathology). It was discovered that until the heat source was within 5mm of the surface of the skin it could not be detected. Now, has infrared technology advanced since then? Absolutely, but have the laws of thermodynamics changed? When asked if these “new” imaging systems have undergone research by reproducing these studies you will find that the answer is no. Until they do there is no proof.
At this point we have something that may be very dangerous. If these claims were true why would we need basic radiology, CT, MRI, ultrasound, mammography, or any other medical imaging technology? Thermography offers significant advantages in many areas, but if patients are allowed to believe that thermography can see deep into the body and provide screening for the early detection of internal disorders we are endangering their lives.
I’ve heard that tooth infections like root canal abscesses can cause breast cancer. Is this true?
No! And this issue needs to be addressed as there are offices who are using this to scare patients into spending thousands of dollars on unnecessary dental procedures and thermograms.
Here are the simple reasons that none of this is possible:
- Due to the Zeroth Law of Thermodynamics, the lymphatic vessels are invisible to thermography.
- No lymphatic vessels lead from the face to the breast.
- The normal immune response does not allow an infection to move all over the body – it walls it off.
- There is no image on a thermogram alone that can be identified as lymphatic congestion or a lymphatic vessel.
Let’s start with the thermograms being seen on the internet. These thermograms show a hot “vessel” or “vessels” leading down from the side of the face, over the front of the neck, and down into the breast. This is assumed to be a lymphatic vessel(s) – error number one.
- All lymphatic vessels drain UP from the breasts. The right breast draining into the right lymphatic duct at the subclavian vein and the left breast draining into the left thoracic duct at the left subclavian vein.
- All the lymphatics from the face drain DOWN and into these same ducts.
- Lymphatics DO NOT drain from the face/head into the breasts.
- What you are seeing on these thermograms are coincidental vein patterns.
- Coincidence does not mean correlation, and correlation does not imply causation.
Lymphatic vessels begin in the tissues as a drainage system for fluid around the cells. All of these vessels travel up from the body below and down from the head above. 90% of these vessels drain into the left thoracic duct, while the remaining 10% drain into the right lymphatic duct. Lymphatics do not drain into the breasts. The lymphatics are a closed system with its own vessels just like the circulatory system.
Another unique aspect of the lymphatic system is that it is completely unlike the circulatory system carrying blood. The pumping heart draws venous blood into it from the body while pushing arterial blood out to the body. The lymphatic vessels have no pump. As such, the flow of lymph (the fluid in the lymphatic vessels) is extremely slow in comparison to the blood circulating through the heart. This last aspect, the flow rate of lymph, is another reason that these vessels are incredibly rare to see on a thermogram.
- In order to see a vessel on a thermogram it must be hotter that the background temperature of the tissues (e.g. skin).
- The Zeroth Law of Thermodynamics basically states that when two objects of differing temperature come in contact with each other they will eventually become the same temperature (they reach equilibrium).
- Since the lymph is coming from the surrounding tissues, the temperature of the lymph is the same as the surrounding tissue.
- The flow rate of lymph through the lymphatics is so slow that the temperature of the fluid remains the same as the surrounding tissue.
- These factors make the lymphatic vessels invisible on thermography.
- The blood flow rate through arteries and veins is fast. As such, the hotter blood moving through the vessels doesn’t have enough contact time with the surrounding tissues to reach equilibrium.
- What we see on a thermogram is the reflection of the blood flow through the skin (i.e. veins and arteries).
What about the root canal infection itself? The human body has evolved to do all it can to survive. The mouth is one of the dirtiest places in the body. Chewing causes tremendous pressures on the teeth and jaws. Due to the importance of having to eat, the mouth is one of the fastest healing areas in the body. Now, let’s introduce an infection. In an effort to survive, what should the body do? Should it wall the infection off isolating it to the tooth area, or should it allow the infection to become deadly by moving to other areas of the body? It does exactly what you just thought, it walls the infection off to fight it and protect the rest of the body. The infection doesn’t pick some specific blood vessel to travel to some specific organ.
Now you might be saying to yourself, “Ok so you can’t see lymphatics. What about the concerns with some people getting heart infections from dental procedures?”. These infections come about from bacteria being dislodged, falling into the venous system, and draining from the mouth – there is no direct connection from the lymphatics to the heart. If the patient has a heart condition that is susceptible to infection (e.g. valve replacement), the bacteria may cause an infection. Keep in mind that bacteria are part of our normal environment both outside and inside our bodies. As such, and if knowing that no recent dental procedures have occurred, an infection of the heart can be coming from anywhere in the body through the venous system.
What about patients with lymphedema? First, there is no vascular pattern (thermal image) that can tell if a patient has lymphedema vs. some other neurovascular condition. As such, for a thermal image to correlate with this diagnosis the interpreting thermologist would need to already know that the patient has this condition (i.e. swollen limb). The accumulation of lymph causes swelling, which is seen on a thermogram as cold – not hot. Again, without the thermologist already knowing the diagnosis this cold image could also be caused by another pathology.
We have also seen statements from dentists and other thermography websites claiming that the teeth are connected to the breast acupuncture meridians. Please feel free to look up any acupuncture meridian chart. There is no such thing as a breast meridian. There are meridians that run through the breast, but there are no breast meridians. Perhaps some are trying to say that the stomach meridian runs directly from the mouth down to the breasts. However, the stomach meridian ends in the feet and not the breast. There is no direct connection.
It is so unfortunate that this topic needs to be addressed, but many patients are being needlessly scared and wasting thousands of dollars on unnecessary dental procedures and added thermograms. There is just no anatomic or physiologic evidence for this topic. A thermogram showing hot stripes from the face to the breast is simply coincidence. A broken clock is right twice a day. Coincidence does not mean correlation, and correlation does not imply causation.
My breast thermogram report mentioned lymphatic congestion.
As mentioned above, there are no thermal patterns or markers of any type that would allow for an interpretation of lymphatic congestion. It doesn’t matter if the image is of the breast, axilla (under arm area), or some other area of the body.
In breast cancer patients who have undergone the removal of a significant number of axillary (under arm) lymph nodes, and have obvious visual proof of lymphedema in the upper extremity, the resulting thermogram of the affected arm would then be a result of lymphatic congestion. However, without knowing the history of this patient, and visually confirming the condition, the interpretation of the upper extremity thermogram would be indistinguishable between some other form of circulatory and/or neurological abnormality.
My report noted “thermal findings indicative of fibrocysts and cysts”.
Interpretations of thermal findings indicating cysts and fibrocysts shows a lack of the basic understandings of thermodynamics. Not to mention the research showing that we can only detect heat sources to a depth of 5mm from the surface of the skin.
You will notice on these types of reports that the interpreter routinely calls attention to “cold areas” or “cold spots” as the location of cysts and/or fibrocysts in the breast. Since cysts are fluid filled sacs, one might think that this area under the skin would create a cold area at the surface. However, simple thermal conduction will not allow for a temperature difference between the cyst and the surrounding tissue. Take for example that a balloon filled with cold water (acting as the cyst) is placed inside a larger balloon filled with warm water (acting as the breast). What will happen over time? Both of the balloons will reach equilibrium and become the same temperature (Zeroth Law of Thermodynamics). This is the same thing that happens with cysts and fibrocysts in the breast. As such, there are no thermal signs of cysts or fibrocysts in the breasts.
The side view of my neck showed carotid inflammation.
This is another example of an inadequate education in thermal imaging. In this instance the interpreting thermologist is looking at a view of the side of the neck and sees a hot stripe leading from the area near the rear of the jaw down toward the front of the neck. This hot stripe is thought to be heat from an inflamed carotid artery.
We have three very elementary errors here. The first is basic anatomy. We have seen websites that state that since the carotid artery is so close to the surface of the skin that it is easily evaluated using infrared imaging. We won’t bore you with an anatomy lesson numerating the layers of muscle, fascia, and other blood vessels that cover and protect this vital structure that conveys blood to the brain. Suffice it to say that the carotid artery is safely located deep in the neck close to the cervical spine. Remember that we cannot see anything deeper than 5mm from the surface of the skin. Secondly, if this heat stripe is a blood vessel how can one prove that it is inflamed only from the thermal image? Simply changing the volume of blood flow will change the size of the vessel; and thus, the appearance of increased heat. And lastly, true carotid inflammation (carotid vasculitis) carries with it a very specific set of symptoms.
So what is this heat stripe? It is the external jugular vein. One of the technical advantages inherent in performing thermography is that a live image is generated. As such, the technician or doctor can approach the patient and investigate the surface of the body for any interesting finding that appears on the live computer image. When seeing this hot stripe, the technician could use a pen to point at an obvious bluish line on the neck (external jugular vein) while looking at the infrared image. The results are obvious.
My report noted “thermal findings over the chest indicating heart problems”.
By now I think you have learned that we cannot see heat coming from the heart through layers of muscle, fascia, and bone. Remember that we cannot see anything deeper than 5mm from the surface of the skin. And by the time a viscerosomatic reflex occurs, creating a thermal signal from the heart, the patient already has obvious cardiac symptomatology. Thermography cannot provide any type of early warning of cardiac disease nor can it rule it out.
I saw an office’s website that mentioned that with their special camera they can offer “privacy imaging” – I won’t need to be undressed in front of a technician.
First, this has nothing to do with the type of camera used. Any office with a reasonable mount for the camera can leave the patient behind a wall or drape and provide imaging without the technician seeing the patient. However, this is not allowed in infrared imaging.
We all understand that we would prefer not to be undressed in front of a technician or doctor. But all of us also understand that when entering any health care facility the likelihood of having to disrobe is fairly high. As mature adults we understand that this can cause some anxiety, but disrobing in front of a technician or doctor of the same gender is something that is fairly common.
The real problem here is that providing imaging without the technician visually seeing the patient is against the standards and guidelines in thermography. It would be irresponsible of the technician not to observe the surface of the body being imaged. During the acclimation process the technician needs to properly position the patient to be sure that thermal artifacts will not be introduced into the images. Once the acclimation time has passed, the technician must re-enter the room to verify that the patient has not changed this position. This is part of the verification of proof of proper acclimation.
When performing breast imaging the technician has special responsibilities that would also preclude “privacy imaging’. Certain changes to the surface of the breast may occur due to surgeries or when a cancerous growth is present. It is the technician’s responsibility to visualize the surface of the breast in order to inform the interpreting thermologist if anything other than smooth uniformly colored skin is present. Surface changes can be critical in the thermal grading of the breast and the proper management of the follow-up recommendations.
With imaging the rest of the body the technician must also be observant for surface evidence of surgical sites (e.g. scars). At times, patients can forget these things when filling out their intake forms. Depending on the extent of certain surgical procedures, the thermal pattern in these regions of the body can be significantly altered. Without having a technician present to observe the surface of the body the interpretation of the thermogram may be in error due to the interpretation of a surgical artifact as a pathology.
It has also been said that many of these things can be overcome by having the patient acclimate in front of the camera in a “privacy imaging” setting. However, one cannot “see” these things in infrared, it’s just not possible. Even if a particular camera was able to provide additional visual imaging just like a regular video camera, you would have to let the patient know that you were looking at them just as if you were in the room. At this point you would be violating the entire “privacy imaging” idea. Decades of experience in thermography has shown that patients do not like having an infrared camera, much less a regular video camera, pointed at them during the acclimation time. It creeps them out.
“Privacy imaging” introduces the possibility of significant errors and violates the standards and guidelines in thermography.
I’ve heard that after my initial thermogram I will need to return in 3 months for another thermogram so that a stable baseline can be established. Is this necessary?
Absolutely not! The argument for this practice seems to be that there is no way to know on your first thermogram whether or not your body was changing at the time. We have another question, if the follow-up 3 month thermogram showed that there was change, which image set would be the stable baseline? Would it be the first set or the 3 month later set? It sounds like you would need to do another set of images in another 3 months as a tie breaker. But what if this set also showed change? The bottom line here is that if you did need to return to do any of this the technology must be useless.
What would you think if your doctor took your temperature, noted it as a fever, and then told you to return the next day to see if this first reading was right? Reading core temperature is no different than a surface recording taken under proper thermal imaging guidelines. Either the information taken on the first thermogram is valuable or the technology is unstable and useless due to some variable in the patient’s physiology. Research following the same patients over a 5 year span has proven that the thermal patterns and differential temperatures at the surface of the body are remarkably stable and held within a very narrow range. These research studies were used to establish the normative database to which patients are compared when reading thermograms. Thermovascular patterns are as unique as a fingerprint and can be followed with accuracy for decades. It is when there is a change to this stable thermal fingerprint that a problem is signaled.
This begs the question as to why patients are being asked to return in 3 months. We recommend asking one of these offices for at least one peer-reviewed and published research paper demonstrating the need for this in order to establish a stable baseline. The research has already been done. In the early days of thermography each set of thermal images were taken in triplicate. The patient was acclimated in a temperature controlled imaging room under standard protocols for 15 minutes and then imaged. The patient would then be left for another 15 minutes and imaged again. This was finally repeated once more. In these early days thermologists were unsure about the stability of the process and the possibility of changes. Once the stability of the thermal data was established this practice was stopped. Then, as mentioned above, this was taken a step further by watching the thermal stability of patients for over 5 years. Studies have proven that a single set of thermal images taken under proper guidelines is completely accurate for analysis.
Under the established standards and guidelines for thermography, recalling patients for follow-up thermograms is based solely on clinical need. When it comes to breast thermography, follow-up thermograms are performed based on the known metabolism of breast cancers. Under these guidelines each breast must be graded into one of 5 thermobiological (TH) categories. The level of TH grading acts as an individualized risk assessment based on the patient’s own biology. Depending on the TH grading, and taking into consideration the metabolism of breast cancers, the patient will be asked to return in a reasonable amount of time.
Since it was established decades ago that a single thermogram is all that is needed for immediate analysis, why are some offices having all their initial thermogram patients return in 3 months?